Keeping well and socially connected
A strong sense of belonging and purpose are key to the health, well-being and quality of life of adults who remain at home and in the community as they age. New models and practices are supporting older adults to remain socially connected and active to the best of their abilities.
Belonging
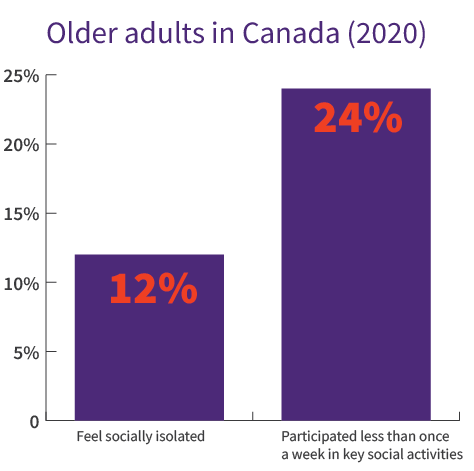
Social isolation is a serious concern linked to a variety of health challenges among older adults, such as depression, cognitive decline and reduced physical activity. Older adults living at home often lose touch with others due to retirement, loss of a spouse or friends, changes in access to transportation and other reasons. The quarantine measures during the COVID-19 pandemic have amplified this risk.
Innovative community responses are making a difference in preventing isolation and loneliness and creating meaningful connections for older adults. Community-based interventions — including drop-in centres, classes, volunteer opportunities and social programs — have been shown to have positive impacts on physical and mental health, a sense of togetherness and personal well-being, quality of life and resilience.
Source: Statistics Canada
Green care farms
The green care movement begun in the Netherlands, which is home to over 1,000 green care farms, engages older adults in farm-related and outdoor activities and gardening. Green Care Farms, a nurturing farm program for people with dementia rooted in purpose and belonging in Canada, offers a design guide to support this approach.
Volunteering
Volunteering helps older adults stay active and connected to their communities, helps maintain social contacts and promotes a sense of value and self-worth. Volunteer Canada has developed tools and resources that explore the opportunities and barriers in engaging older adults in giving.
Men’s Sheds Canada
Men’s Sheds are modern, shared versions of home workshops — a gathering place for men to contribute to society and connect over activities such as woodworking, cooking and music. The Canadian Men’s Sheds Association is a peer-run group that aims to build relationships between Canadian sheds, help new ones get started and raise awareness about the friendly, inclusive and creative spaces that sheds can offer.
Intergenerational programs
Bringing young people and older adults together online or in person for shared interests reduces isolation, promotes community and helps to combat ageism. Programs include online and in-person activities such as visits and walks, art experiences, storytelling and oral histories, learning activities and health supports. Guides are available to support individuals and organizations who wish to set up intergenerational programs.
Volunteer Grandparents, Canada
Intergenerational Society, Canada
Social prescribing
Social prescribing is a holistic approach that creates a formal way for health providers to address a wide range of key social, health and wellness needs by writing a prescription. Older patients are referred to connectors, health advisors, co-ordinators, care navigators or community navigators who provide links to needed services. These can include bereavement support, creative arts, nature-based activities, gardening, museum-based activities, lunch clubs and walking clubs, among other activities.
From 2018 to 2020, the Alliance for Healthier Communities implemented Rx: Community — Social Prescribing, the first-in-Canada social prescribing research project. Emphasizing the importance of an asset-based approach, navigators worked with each individual to provide social prescriptions that highlighted their unique goals and gifts. For more information, watch the video or see this overview.
Helpful resources
Efforts targeting social isolation — often grassroots in nature — come in all shapes and sizes. If you’re interested in exploring more, these resources provide some models, principles and practical tips.
Nelson Allen Toolkit: Supporting designing community-based approaches
Innoweave: Offering social innovation tools and coaching to support community organizations in designing change
The Social Medicine Program at UHN: Working alongside community organizations, clinicians, patients and others to co-design innovative programs for better health
Promising Approaches Revisited: Effective Action on Loneliness Later in Life: Offering a framework for an effective community response (UK Campaign to End Loneliness)
Physical activity
Physical activity is a key factor in helping older adults maintain the ability to live at home. Tai Chi, group and home-based exercise programs — usually containing some balance and strength training — are effective in reducing falls. Peer-led community programs help promote general health and physical functioning, and resources from organizations promoting physical activity help older adults focus on achievable goals and outcomes.
Choose to Move at Home,
Active Aging SocietyTips to Get Active,
Public Health Agency of CanadaMake Your Day Matter: 24-Hour Movement Guidelines 65+,
Canadian Society of Exercise Physiology

Self-management
Self-management programs can help older adults remain in their homes by improving their ability to carry out daily activities and manage declines in their health. As a supplement to professional medical care, they can take various forms — such as information, communication, education, training, coaching and personal health plans. The World Health Organization’s innovative Be He@lthy, Be Mobile uses digital technology to help older adults self-manage at home and prevent decline through texts that encourage healthy and helpful actions and behaviours.
Designing the future
Community-based and system efforts to promote social connection, physical activity and self-management are key to better aging. Canada’s National Seniors Council identified the following key ingredients in programs that successfully combat social isolation in older adults.
Types of programs
Group
One-on-one
Arts and culture
Leisure
Intergenerational
Educational
Friendship
Telephone support
Gatekeeper programs
Internet groups
Religious
Support-provision and groups
Characteristics of programs
Are based on sound theory
Involve older adults throughout
Include members who share a common interest
Directly target social isolation and loneliness
Use more than one intervention
Train and support staff
Activate community-based resources
Mobilize nurses and other health professionals as champions and gatekeepers
-

What helps?
• Involving older adults. Models that involve older adults in co-creation, planning, implementation and evaluation are more successful. Considering the specific needs and preferences of segments of the population (e.g., newcomers) is key in reducing social isolation.
• Offering a variety of options. Models and tools that provide a range of offerings and choice in format and delivery — and the ability to cater to the interests and needs of a given community — have greater potential to succeed.
-

What hinders?
• Ageism. Ageism is associated with increased social isolation and loneliness in older adults. The WHO’s Global Campaign to Combat Ageism offers a toolkit to learn about ageism and organize events to raise awareness.
• Change readiness. Innovative models that incorporate changing roles for providers and older adults can encounter practical and psychological barriers. These include concerns about quality referrals, liability and workload from clinicians and lack of confidence and motivation from older adults in participating.
Food for thought
Social isolation is defined as “low quantity and quality of contact with others.” In trying to create a greater sense of belonging for older adults in your community, would you focus on improving quantity or quality of contact — or both? Why?
Based on what we know about the early warning signs and risk factors of social isolation, what practical steps might your community take to help identify, prevent and protect older adults against social isolation?
How might we enable participation for older adults who live in areas lacking local events and activities?
How ready is your community for social prescribing? What factors do you think are important to have in place for this approach to be successful?
As an older adult, what additional supports might help you better manage, on your own terms, the challenges you face as you age in your home?
Additional resources
The Path Forward for Aging in Canada discussion paper
Articles
Many seniors struggle with loneliness. The pandemic has only made it worse (Global News Alone and Apart series, 2020)
The cost of loneliness: Canadians are facing a solitary future — and it's affecting their health (Ottawa Citizen, 2019)
How promoting social connection could help combat suicide among rural men (CBC The Current, 2020)
In a Time of Crisis, a City Fights Isolation (The New York Times, 2021)
Loneliness in Seniors: Understanding Its Impact and Ways to Help (Closing the Gap, 2020)
“Adopt a Grandparent” program sees influx of virtual volunteers from across the globe (Good Morning America, 2020)
Simple tips could help more aging Canadians to live at home independently (CBC, 2021)
Why your retirement years are the best time to get fit (Globe and Mail, 2021)